by fopindia | Oct 4, 2018 | Uncategorized
Blueprint Medicines Corporation, a leader in discovering and developing targeted kinase medicines for patients with genomically defined diseases, today announced preclinical proof-of-concept data for BLU-782, an investigational oral precision therapy specifically designed to target mutant activin-like kinase 2, the underlying cause of fibrodysplasia ossificans progressiva. Preclinical studies in a well-characterized, genetically accurate FOP model showed BLU-782 prevented injury- and surgery-induced heterotopic ossification, reduced edema and restored healthy tissue response to muscle injury. The data were presented on September 30 in a plenary oral session at the 2018 American Society for Bone and Mineral Research Annual Meeting in Quebec, Canada.
“We are excited to report preclinical proof-of-concept data for BLU-782, a highly selective oral inhibitor of mutant ALK2, the underlying cause of FOP,” said Marion Dorsch, Ph.D., Chief Scientific Officer of Blueprint Medicines. “Despite the discovery of the FOP gene more than a decade ago, prior efforts to develop a selective ALK2 inhibitor faltered due to persistent technical challenges. By leveraging our proprietary compound library and expertise in structure-guided medicinal chemistry, we overcame these challenges and successfully designed BLU-782 to selectively target mutant ALK2. The new preclinical data reported at the ASBMR Annual Meeting showed BLU-782 prevented abnormal bone growth in a well-characterized FOP model, validating selective ALK2 inhibition as an important potential therapeutic strategy.”
FOP is a rare genetic disorder characterized by the abnormal transformation of skeletal muscle, ligaments and tendons into bone, either spontaneously or as the result of physical trauma. FOP is caused by a mutation in the gene for ALK2, which is known as ACVR1, that causes hypersensitivity to certain bone morphogenetic proteins (BMP) and a neomorphic response to activins.
In the preclinical data presented at the ASBMR meeting, BLU-782 demonstrated exquisite selectivity for R206H mutant ALK2 in cellular assays, while sparing closely related anti-targets including ALK1, ALK3, and ALK6. Additionally, BLU-782 potently inhibited mutant ALK2 in vitro, regardless of the activating ligand, including Activin A, Activin B and BMP6. In vivo studies in a conditional knock-in ALK2R206H transgenic mouse model showed BLU-782 prevented the formation of injury-induced HO and edema, as measured by micro computed tomography and magnetic resonance imaging. Immunohistochemistry analyses also showed restoration of a healthy response to tissue injury in ALK2R206H mice, including skeletal myofiber regeneration. In addition, BLU-782 prevented the formation of surgery-induced HO following fibular osteotomy surgery in ALK2R206H mice.
“Given the disabling and destructive nature of this disease, people living with FOP have a desperate need for a safe and effective treatment,” said Adam Sherman, Research Development and Partnerships Director at the International Fibrodysplasia Ossificans Progressiva Association. “We are immensely grateful to have companies like Blueprint Medicines developing new treatments for those living with FOP. We look forward to seeing BLU-782 advance through the development pathway and hope a therapeutic option will one day change the course of this disease.”
Blueprint Medicines expects to submit an investigational new drug (IND) application for BLU-782 by the end of 2018, and subject to approval of the IND application by the U.S. Food and Drug Administration, plans to initiate a Phase 1 clinical trial in healthy volunteers in the first quarter of 2019. In addition, Blueprint Medicines plans to continue working with clinical experts and the patient community to design a potential Phase 2 clinical trial of BLU-782 in patients with FOP.
Source: Blueprint Medicines

by fopindia | Oct 4, 2018 | Uncategorized
Clementia Pharmaceuticals Inc., a clinical-stage biopharmaceutical company innovating treatments for people with ultra-rare bone disorders and other diseases, today announced updated data from the open label extension (“Part B”) of its ongoing Phase 2 clinical trial of palovarotene in fibrodysplasia ossificans progressiva (FOP).
“These updated data continue to support the potential for palovarotene in FOP, an ultra-rare and devastating bone condition,” said Clarissa Desjardins, Ph.D., founder and chief executive officer of Clementia. “Twelve-week flare-up outcomes for patients treated with palovarotene in our Phase 2 trial indicate a consistent treatment effect of approximately 73 percent reduction in mean new bone growth, or heterotopic ossification, and palovarotene was generally tolerated in both adult and pediatric patients. However, we observed that nearly half of the patients in Part B had flare-ups that went untreated mainly due to the criteria for flare-up treatment specified in the Part B protocol. The flare-up treatment criteria in the MOVE Trial, on the other hand, are expected to result in more frequent use of flare-up up dosing in response to flare-up symptoms. First and second interim analyses from the MOVE Trial are expected to occur in the second and third quarters of 2019, respectively, and are designed to assess new HO in treated patients as compared to external natural history study controls. We look forward to those data readouts next year and anticipate that they’ll reflect the true potential of palovarotene in patients who urgently need a treatment option.”
Updated 12-Week Flare-up Imaging Results
The final set of 12-week flare-up imaging data were presented today in a poster session at the Mechanistic and Therapeutic Advances in Rare Skeletal Diseases, a meeting organized by the Rare Bone Disease Alliance in association with American Society of Bone and Mineral Research (ASBMR), and will also be presented on Monday, Oct. 1, 2018 in a poster session at the ASBMR 2018 Annual Meeting (Presentation Number: MON-1066). The data demonstrate a consistent greater than 70 percent reduction in new heterotopic ossification (HO, or bone growth in abnormal places) across three different dosing regimens, as detailed below:
| Treatment group |
N= |
Volume of new HO (mm3) at 12 weeks |
% reduction |
p=value1 |
| Placebo/untreated |
46 |
11,014 |
– |
– |
| Palovarotene 10/5mg |
46 |
2,731 |
-75% |
p=0.05 |
| Palovarotene 20/10mg |
15 |
3,045 |
-72% |
p=0.02 |
| Palovarotene chronic / flare-up |
31 |
3,018 |
-73% |
p=0.16 |
1ANOVA with BCa bootstrap and covariate adjustment
The poster also presents details on 12-week flare-up outcomes at the hips and shoulders, the two most frequent flare-up locations, and flare-ups at these locations result in substantially more bone than flare-ups at other locations. The treatment effect for flare-ups that had any new HO at these locations at 12-weeks varies between 60 and 97 percent reduction in new HO, depending on the treatment regimen.
As previously reported, palovarotene is generally tolerated in our ongoing Phase 2 study. There were dose-related increases in retinoid-associated adverse events (AEs) with most being mild or moderate in severity, and only one patient discontinued participation in the study because of an AE. There were no treatment-related effects on laboratory or ECG findings or on skeletal growth in pediatric patients.
Updated 12-month Whole-body CT Scans (WBCT)
In addition to the data presented in the poster, the company announced updated WBCT data that demonstrate new HO at 12 months in the palovarotene treated per protocol group of 23,335 mm3, a reduction of 3,639 mm3, or 13 percent (n=33, p=ns), versus the 26,974 mm3 new HO volume observed in untreated NHS patients (n=58). Updated review of the data indicates that 47 percent of patients (n=15) had flare-up symptoms that were either untreated or under-treated. Due to the narrow definition of a flare-up in Part B, which required at least two flare-up symptoms and did not allow for flare-up dosing in connection with intercurrent flare-ups, these patients did not receive the 20/10mg regimen for their flare-up symptoms. These patients exhibited a mean new HO of 39,443mm3. In those patients who did receive the 20mg/10mg regimen (n=9) for all reported flare-ups, the mean volume of new HO was 1,787mm3, a 93 percent decrease versus untreated patients.
Clementia believes that the flare-up treatment definition in the ongoing MOVE Trial is expected to result in more frequent use of flare-up dosing in response to flare-up symptoms. Preliminary treatment rates (treated flare-ups per subject month exposure) from the MOVE Trial support this assessment, as the treatment rate in the MOVE Trial is much higher than that observed in our Part B study. As a result of this, the company does not believe that the Part B WBCT data are a reliable predictor of potential outcomes in the MOVE Trial.
Source: West
by fopindia | Oct 4, 2018 | Uncategorized
Human skeletal stem cells that become bone, cartilage, or stroma cells have been isolated from fetal and adult bones. This is the first time that skeletal stem cells, which had been observed in rodent models, have been identified in humans. The researchers were also able to derive the skeletal stem cells from human induced pluripotent stem cells, opening up new therapeutic possibilities. The discovery appears September 20 in the journal Cell.
“Given the tremendous medical burden imposed by degenerative, neoplastic, post-traumatic, and post-surgical skeletal disorders, we believe that identifying this human skeletal stem cell and elucidating its lineage map will enable the molecular diagnosis and treatment of skeletal diseases,” says senior study author Michael Longaker of Stanford University School of Medicine.
Skeletal tissues such as bone possess exceptional regenerative potential. Bone defects heal readily, and some vertebrates can regenerate entire portions of their limbs. But the regenerative capacities of skeletal tissues in other vertebrates are more restricted. For example, bones in mice and humans can recover from small- to moderate-sized defects, but adult cartilage tissues possess little to no regenerative ability. In addition, both mice and humans display severe age-related degeneration of skeletal tissues over time.
Skeletal dysfunction can lead to a broad spectrum of health conditions ranging from age-related diseases such as osteoporosis and osteoarthritis to non-healing skeletal injury, blood disorders, and even cancer. Despite its significant impact on health and disease, treatment options aimed at improving skeletal function are currently limited. One major hurdle is that stem cell regulation in the human skeletal system remains largely unexplored.
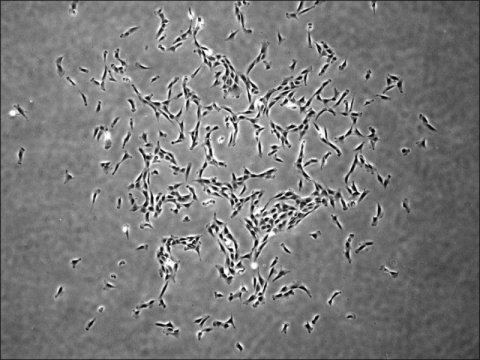
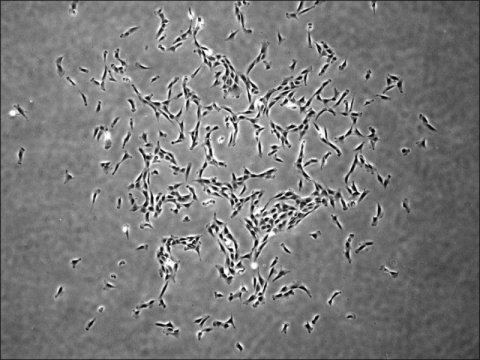
In the new study, Longaker and his collaborators addressed this gap in knowledge by identifying and characterizing human skeletal stem cells and downstream bone and cartilage progeny in a variety of tissues. These self-renewing and multipotent cells were present in both fetal and adult human bone marrow tissues and could be derived from induced pluripotent stem cells (iPSCs). By defining the relationships between human skeletal stem cells and downstream skeletal progenitors, the researchers created a detailed lineage map of stem-cell-mediated formation of skeletal tissues in humans.
Moreover, transcriptomic and epigenetic comparisons with mouse skeletal stem cells revealed evolutionarily conserved pathways regulating the stem-cell-mediated formation of skeletal tissues, as well as divergent molecular pathways that may regulate species-specific differences in bone development and skeletal structure.
“By comparing the molecular and functional differences in specific types of stem cells between different species of vertebrates, it may be possible to uncover convergent and divergent mechanisms that underlie tissue growth and regeneration and apply this understanding towards enhancing health and rejuvenation in humans,” says first author Charles Chan of the Stanford University School of Medicine.
Source: ScienceDaily

by fopindia | Oct 4, 2018 | Uncategorized
Learn more about Regeneron’s LUMINA-1 clinical trial presented by Dr. Richard Keen from the Royal National Orthopaedic Hospital in England. This webinar is hosted by FOP Friends in the United Kingdom http://fopfriends.com/.
Source: FOPnews